In a significant proportion of children presenting with a first afebrile seizure no diagnosis is found.
Differential diagnoses
1st presentation epilepsy
Acute symptomatic seizure i.e. related to:
- Intracranial infection
- Ingestion
- Trauma
- Tumour
- Intracranial haemorrhage
- Hypertension
- Hydrocephalus
- Metabolic (low glucose/ calcium/sodium etc)
In children under 3/12 in addition to the above the following diagnoses are considered-
- Hypoxic Ischaemic Encephalopathy (from birth)
- congenital infection
- Fifth day fits
- Drug Withdrawal
- Pyridoxine dependancy
Other important differentials
Convulsive syncope:
- Reflex anoxic seizures
- Vasovagal seizure
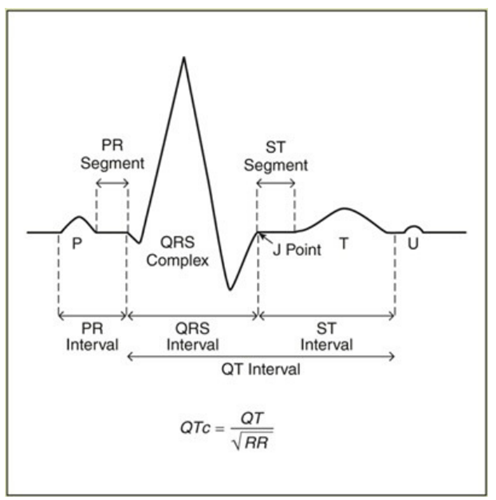
- Arrythmias e.g. long QT syndrome
- Suffocation
- Psychogenic seizures