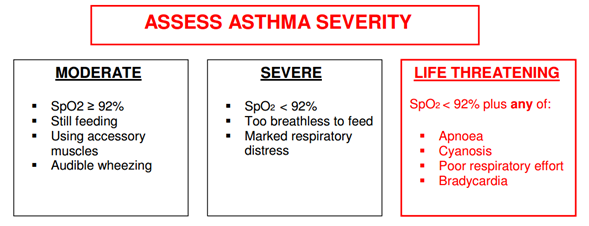
- If a patient has symptoms and signs across categories, always treat according to their most severe features
- Most infants have recession with audible wheeze but are not distressed
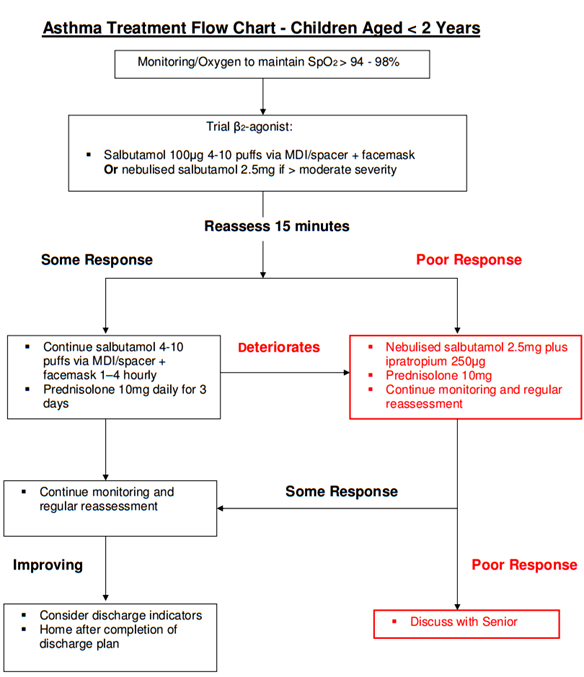
- MDI + facemask/spacer is as effective as, if not better than, nebulisers for treating mild to moderate asthma in children aged < 2 years
- Steroid tablets in conjunction with β2-agonists have been shown to reduce hospital admission rates when used in the ED
Acute Asthma Management, Children Under 2 years, Emergency Department, Paediatrics (334)

Objectives
The diagnosis of acute asthma in early childhood can be difficult. Intermittent wheezing attacks are often due to viral infection and the response to asthma medication is inconsistent. The differential diagnosis of wheeze in this age group includes pneumonia and bronchiolitis.
The possibility of an underlying congenital anomaly or chronic condition should also be considered.
These guidelines are intended for those children < 2 years who are thought to have asthma causing acute wheeze. They should not be used as a guide for treating bronchiolitis/other conditions.
Scope
This guideline should be used by healthcare professionals involved in the care of children less than two years of age that have acute asthma.
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
Based on British Thoracic Society, Scottish Intercollegiate Guidelines Network British Guideline on the Management of Asthma. 2009 revision[1]
|
Prescribing prednisolone for patients being admitted to the wards with acute asthma:
|