Ultrasound
Undiagnosed cases are associated with more complications and significant morbidity; a high level of suspicion in women with previous sections and a low anterior placenta is required. Women with other uterine surgery should also prompt careful assessment of the placenta. These operations may be elsewhere in the uterus.
Risk Factors:
- Caesarean section
- Myomectomy
- Hysterotomy
- Endometrial Ablation
- Uterine Perforation
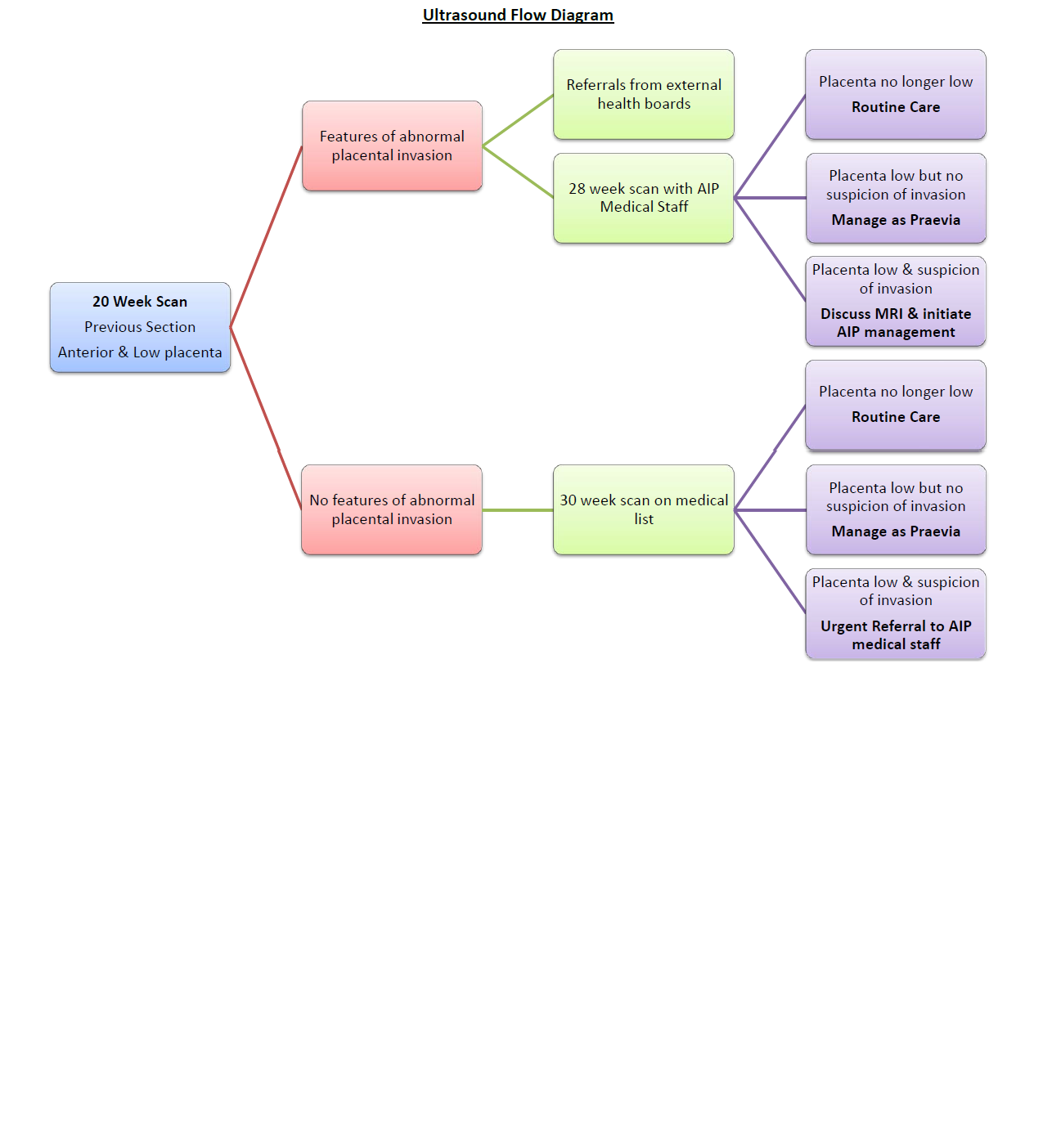
20 week ultrasound may show anterior low placenta with a previous section. If there are no suspicious features then repeat sonographer scan at 30 weeks. If placenta remains anterior and low at 30 weeks with or without features suspicipous of invasion a medical scan should be arranged.
If suspicious features are already present then a 28 week scan with a medical AIP sonographer should be arranged. See the flow chart below for management plans.
It is anticipated that referrals from external health boards may present at this stage. These women should have been scanned by a medical sonographer in their own unit and be referred directly to one of the AIP consultants at around 30 weeks. One of the AIP medical staff will then arrange an ultrasound scan to assess their placenta.
In women with a confirmed ultrasound diagnosis further imaging with MRI can provide useful information to help plan surgery. Please see the flowchart and MRI criteria in this document.
Abnormally Invasive Placenta - Ultrasound Assessment Form
Magnetic Resonance
- A referral for MRI of the placenta (TRAC request MR Obstetric) should be made only after a possible or probable risk of AIP is raised by one of the AIP medical sonographers triggering entry of that patient onto the AIP pathway. This referral for MRI will probably be at 30 weeks.
- The referral for MRI should be to a named radiologist at the site of referral; they should also be contacted by e-mail- see list below
- The referral information should include
- A link to USS images if possible and/or a list of the specific, positive USS findings (copy of USS proforma shown in guideline included in request or on Portal). This information should include the site of concern and totalled estimated risk score and features on ultrasound.
- EDD, parity, number of previous LUSCS.
- Consideration of MRI contraindications.
- An MRI scan will be appointed at the site of referral.
- The MRI scan can be performed to the agreed local GGC imaging protocol and will ideally be reviewed and reported by 2 radiologists.
- MRI is adjunctive and complementary to USS and should not be interpreted or acted upon in isolation.
- MDT discussion for patients on the AIP pathway is advised to discuss the salient USS and MRI imaging findings with the surgical, obstetric and pathology team to guide subsequent management and interpretation.
- Surgical, IR, pathological and medical photography feedback to radiology in ALL cases in the first instance to Emily.Stenhouse@ggc.scot.nhs.uk
If the diagnosis of AIP is confirmed or seems likely then progress to the management section; otherwise manage as other placenta praevia cases. (see praevia guideline )