Parvovirus Guideline (593)
| Please report any inaccuracies or issues with this guideline using our online form |
Parvovirus B19 virus responsible for erythema infectiosum (fifth disease/ slapped cheek syndrome), 50-75% women of reproductive age are immune.
There is no specific treatment or prophylaxis available against B19 infection, but counseling of non-immune mothers and active monitoring of confirmed maternal infections with intervention to correct fetal anemia is likely to decrease mortality. At present there is no vaccine or treatment with immunoglobulin available.
Spread by respiratory droplets or hand to mouth contact. Epidemics can occur spring and mainly affects children. Viraemia occurs 4-14 days after exposure. “Slapped cheek” rash occurs 1-4 days and is associated with appearance of parvovirus B19 IgM antibodies.
Signs and Symptoms, Mild fever, flu like symptoms, slapped cheek rash, arthralgia. Up to 70% of infected pregnant women are asymptomatic.
Fetal Effects of Parvovirus
This can lead to spontaneous miscarriage and stillbirth. Spontaneous loss before 20 weeks is 13% and after 20 weeks is 0.5%
Incidence of hydrops fetalis is 3%. Positive parvovirus infection in the absence of hydrops or anaemia does not seem to cause long term neurological morbidity. There is no increase in congenital abnormailty. The peak risk is 5 weeks post infection (range 2-12).
Exposure/Infection
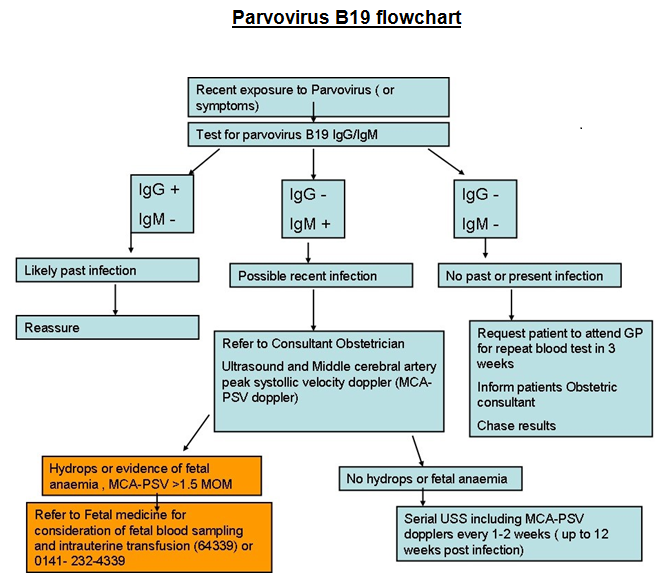
If a woman is exposed to or develops signs or symptoms of parvovirus check immunity
- Request IgM ( current) and IgG ( past ) antibodies from booking blood virology
Contact Laboratory: 211-0080 (50080)
- If not yet had booking bloods then should attend GP ( NOT to attend maternity unit due to risk of infection)
- Email/ contact patients named Consultant informing of test, chase result.
IgM appears after 2 weeks and may last 4 months. IgG appears after 3-4 weeks and lasts for life
IgG + means immune ( previous parvovirus)
IgG – means not immune (susceptible to parvovirus )
IgM + means infected ( has current infection- needs action)
IgM – means not infected ( no current infection)