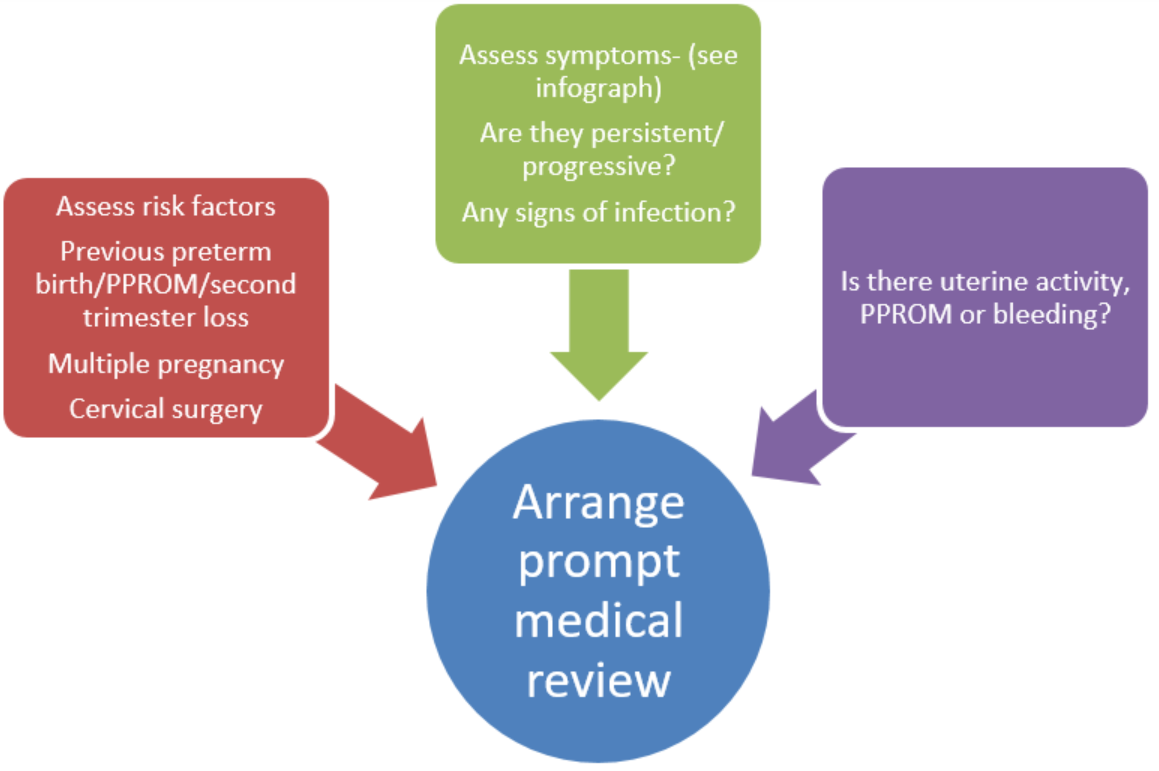
Women can experience a range of subtle and non-specific symptoms during the prodromal period leading up to pre-term labour. These symptoms can develop over days to weeks prior to established pre-term labour(3).
Although with low predictive value, these symptoms cause women to present themselves to health care services providing the opportunity for early diagnosis.
Signs and symptoms may include (4) (Please refer to attached infograph)
- Abdominal Cramps- with or without diarrhoea
- Backache- low, dull constant
- Contractions
- Vaginal Discharge (increase in the amount of discharge) or bleeding
- un-Easiness- feeling “not right”
- Fetal movements /urine Frequency– changed
- Gush of fluid loss - preterm rupture of membranes
- Heaviness or pelvic pressure—the feeling that the baby is pushing down
Subtle changes in uterine activity patterns have been detected a few days to several weeks before overt pre-term labour (5). Uterine activity may or may not be perceived by patients at all and are not necessarily painful. It has been observed that only about half of women can feel painful uterine activity in the days preceding pre-term labour. About a third of patients can report no uterine contractions (3). One in five patients admitted with suspected pre-term uterine activity go on to develop established pre-term labour.