The Scottish Ambulance Service (SAS) Trauma Triage Tool (TTTT)
Triage is the process of sorting patients by urgency and priority. It is a dynamic process and should be reassessed at multiple points. There is a nationally agreed SASTTT, both adult and paediatric, in the pre- hospital arena to decide the initial destination of the patient. This should initially be applied by SAS to determine suspected major trauma patients. The majority of suspected major trauma patients in Scotland will undertake primary transfer including bypassing nearby hospitals to the MTC. However, in the north of Scotland, due to the geography, the majority of transfers will take longer than 45 minutes to reach the MTC and many major trauma patients will be taken to an LEH or the TU if resuscitation is required before then being transferred to the MTC.
Defining suspected major trauma patients
Major Trauma patients are often only defined days after their injury, when their injury severity score (ISS) has been calculated as >15. This document uses the term Major trauma patients to encompass any patient taken to a TU or MTC who is suspected to have suffered Major Trauma based upon a triage tool or clinical judgement, regardless of their eventual ISS score.
Defining secondary transfers
Type of transfer |
Definition |
Examples |
Notes |
| 'Hot' time critical | Life or limb threatening injury has been mis-triaged, self presented or diverted to TU. | Uncontrollable haemorrhage, ischaemic limb, intracranial bleed with mass effect, post thoracotomy. |
Patient should leave within 30 minutes. If transfer imminent leave on scoop and transfer with initial ambulance. Otherwise book a blue light priority (<8 minutes) when patient being packaged to leave. |
| Urgent | Require MTC care though not in imminent danger. | Non limb threatening open long bone fractures. | Ambulance to arrive within 1 hour of booking. Usually ED to ED. |
| Non urgent secondary | Isolated speciality injuries. | Pelvis fractures, stable ICU patients. | Transfer to occur within 24 hours of decision to transfer. Usually ward/ICU to ward/ICU. |
Key principle – automatic patient acceptance
Automatic patient acceptance to the MTC is a fundamental principle of the network. If a phone call is made about the need to transfer a critically injured patient, the patient is accepted. Critical care bed availability in the MTC is not a pre-requisite for automatic acceptance. The MTC trauma team leader (TTL), using the Single Point of Contact, should be called by the TU/LEH to notify them of the patient and allow the MTC to make preparation for their arrival. The SAS will still place a 15-minute pre-alert call stating trauma unit transfer with the standardised ATMIST handover. The following patents may be transferred under automatic acceptance criteria though these are by no means mandatory criteria:
- See separate TBI transfer guideline
- Major vessel injuries
- Flail chest
- Crushed, de-gloved, mangled, or pulseless extremity
- Amputation proximal to wrist or ankle
- Pelvic fracture with haemodynamic instability
- Paralysis
- Multi-system injuries and a suspected ISS>15
- Grade III or above solid Organ that may require Interventional Radiology
- High energy open long bone fracture (as decided by senior Orthopaedic surgeon)
- Post Damage Control Surgery performed at TU
- TU TTL believes the patient would benefit from MTC care.
Even if a patient fits the above criteria, it is still permissible for the patient to remain in TU care if this is deemed appropriate by the TU TTL. Similarly, the TU TTL consultant may wish to discuss with the MTC TTL at consultant level the suitability of transfer of certain major trauma patients, where remaining at the TU may be more appropriate. Examples may include:
- Patients with a DNACPR, advance directive with major injuries where interventions may not be appropriate.
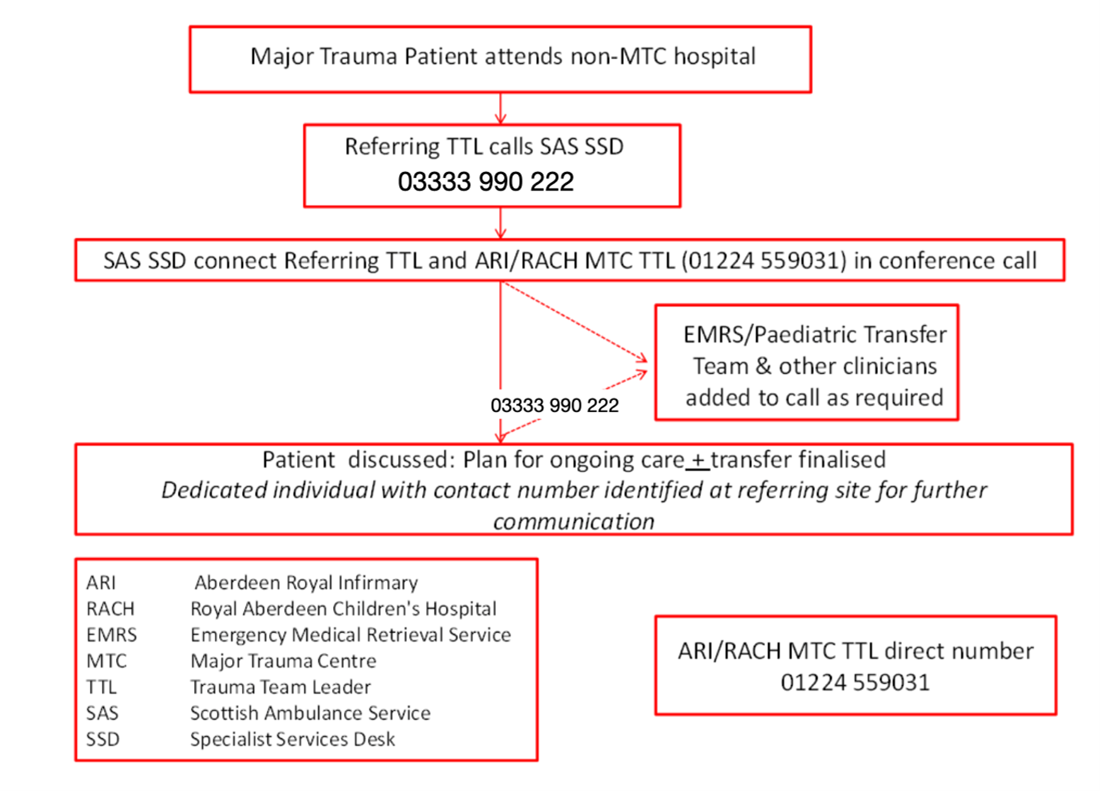
Transfer algorithm
The process for undertaking TU/LEH to MTC transfers is detailed in the algorithm below and the detailed SOP.
Responsibility for transfer
Once the decision to transfer the patient and contact has been made with the MTC SPOC, it remains the responsibility of the TU and LEH Trauma Transfer Lead to determine the appropriate person and equipment to undertake the transfer (using the transfer checklist). The escorts should have appropriate training and skills to manage the patient during the transfer, be familiar with equipment and process surrounding the transfer of critically ill or injured patients.
- For intubated patients, the following specialties include transfer training in their curricula:
- Anaesthesia
- Intensive care medicine
- Pre-hospital emergency medicine.
For non-intubated patients, the TU/LEH TTL must decide if an escort is necessary, or the patient can be transported with SAS and no escort. If an escort is necessary, the TU/LEH TTL should decide on the most appropriate person. Escorts are not routinely required so only consider if specific complications are expected. These decisions should consider the severity of injuries, ongoing treatment, and staffing levels in the TU/LEH SAS will not routinely return the team to their base hospital.
