Treatment of electrical injuries algorithm (pdf for printing)
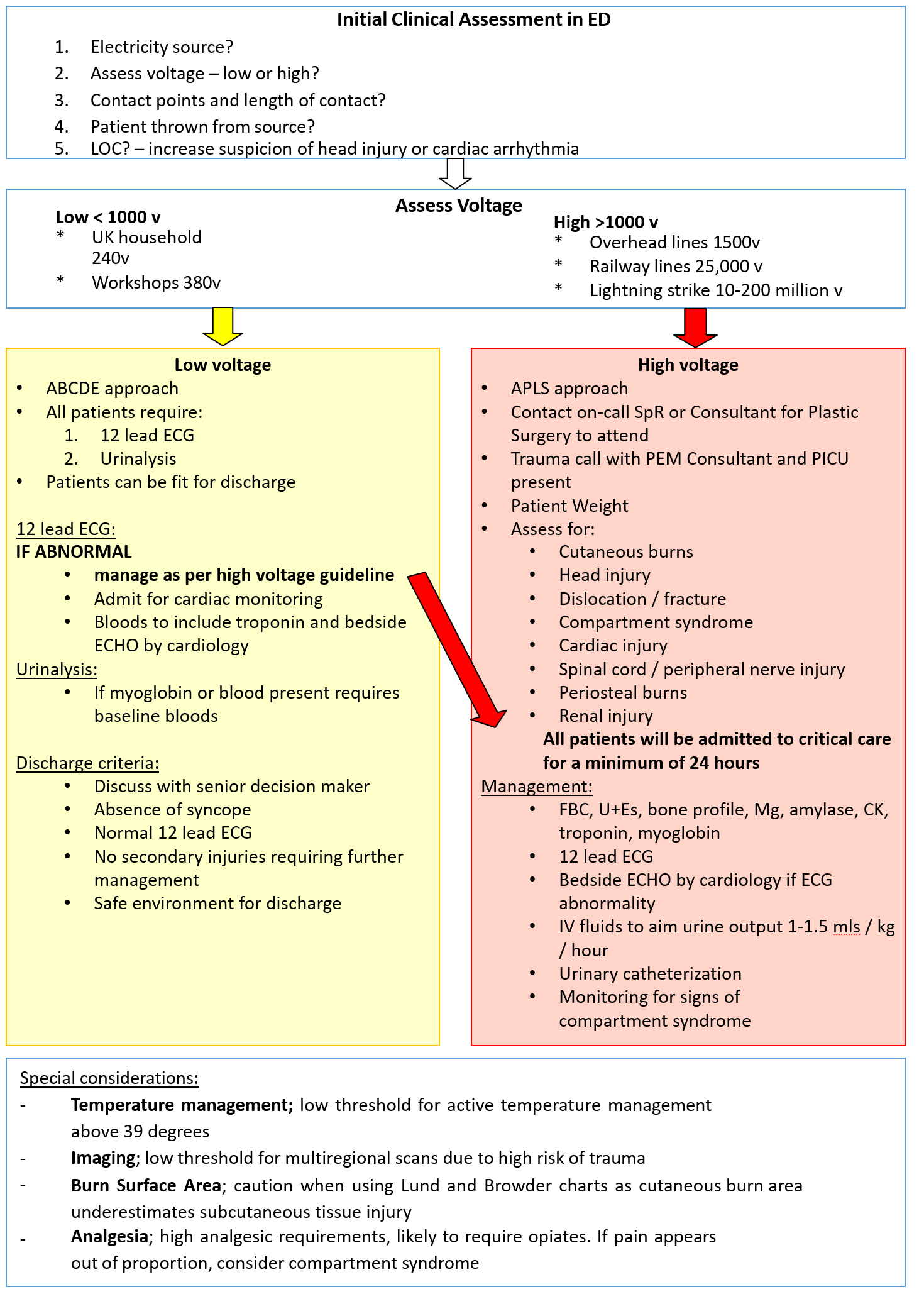

Guidance for the assessment and management of electrical injuries in children and young people under 16
Medical and nursing staff caring for children presenting with electrical injuries. Emergency Medicine, PICU, Plastic Surgery, Cardiology
Presentation with electrical injury is rare and depending on the underlying voltage, injures can range from small cutaneous burns to significant internal organ damage and musculoskeletal injury.1 In the paediatric population 2 age peaks are seen; children under 6 years and adolescents aged between 13 to 18 years.1, 2
Significant injuries are known to occur even in the absence of large burns or other obvious signs of external or internal injury.
A systematic literature review was performed to identify international standards and current clinical guidelines.3, 4, 5
ABCDE approach – unless suspicion of trauma
12 lead ECG – if abnormal follow management of high voltage injury- will require admission
Assessment and treatment of burns as per burns guideline (Note: Assess for burns at oral commissure in children – risk of sublingual haematoma)
Low voltage injuries can be considered for discharge if;
*If does not meet above criteria discuss with senior decision maker for admission*
C-SPINE IMMOBILISATION
High index suspicion for spinal cord injury (convulsions/fall)
AIRWAY + BREATHING
Supplemental oxygen
Early senior anaesthetic review and consider intubation (uncut tube) if evidence airway burns
CIRCULATION
12 Lead ECG- non-specific ST changes, AF, VF/VT, asystole
Bedside ECHO if ECG abnormal
Continuous ECG monitoring
IV access and bloods – FBC, U+Es, bone profile, Mg, CK, troponin, myoglobin
IV fluid resuscitation - 0.9% NaCL target 1-1.5ml/kg/hr urine output
Urinary catheterisation
DISABILITY
GCS and hourly neuro obs
If GCS reduced consider head trauma, anoxia from arrhythmia, effect of electricity on brain
EXPOSURE
Assess extent of cutaneous burns – manage as per burns guideline
Full exposure including soles of feet and palms, looking for entry/exit points
Assess extremity injuries- fractures/dislocations
Assess for compartment syndrome – immediate plastics involvement for consideration of fasciotomies
Careful temperature management- low threshold for active temperature management above 39 degrees
Imaging as indicated by findings of primary survey (note: small and large bowel most injured viscera with risk of abdominal compartment syndrome)
All require admission
For 24hr monitoring in Critical Care
Echo if not required in ED
6 hourly electrolytes/creatinine/CK
For all cases, regardless of high or low voltage injury, consider whether there is concern for the welfare of the child, whether there was suitable supervision, whether there is concern of future harm. If in doubt as to whether completing a notification of concern is appropriate please seek advice from a senior member of staff.