Learning to feed is an important milestone for your baby. Most full term babies are able to feed right from birth but preterm babies or sick babies may need special help as they learn to feed. Cue based feeding means that we use your baby’s cues to help us to know when your baby is ready to start feeding, and how to progress their feeding. During the feed we will also watch for cues that tell us when baby wants to stop feeding.
To start with your baby may only manage to suck small amounts so the rest will be given through the feeding tube.
Cue based feeding also helps us keep track of how well your baby is feeding (the quality of feeding), and how your baby’s feeding is progressing.
Cues are your baby’s way of talking to us. Your baby talks to us through changes in his or her behaviour - facial expressions, breathing, posture, movement and wakefulness.
Your baby’s cues and medical needs help guide the feeding and will change as your baby learns and grows. The amount your baby sucks is important, but the quality of feeding is more important. A successful feed is a safe and enjoyable experience for both baby and parents, and one that matches your baby’s individual stage of development
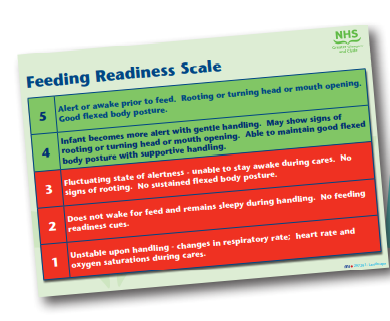
Feeding Readiness Scale and When to Stop The Feeding Readiness Scale is used to assess what your baby’s feeding cues mean, and to know when it is right to offer your baby a suck feed. We will show you how to match your baby’s cues to a score. The feeding cues are assessed before each feed.
The score will tell you whether baby should be offered a feed or should have their milk through their feeding tube. The scores are 1-5. If baby scores a 4 or 5 then it is safe to offer baby a suck feed. A score of 1, 2, or 3 tells us that baby should be given their milk through the feeding tube. There will always be a nurse to guide you.
It is important to respond to baby’s cues and allow them to suck, even in the early stages when they may only suck for a short time. They are telling us that they are only ready for a short feed - they stop when their need is satisfied or they become tired but it is important that they are given the opportunity to suck when they are ready.
We will also show you how to recognise cues and signs that will tell us when to stop feeding. It is very important that you do not to try to encourage your baby to feed when they are showing STOP signs. Encouraging can tire baby and they will not enjoy feeding. It may cause them to be reluctant to suck at the next feeding time and can delay baby’s progress. The Scale Charts are on the wall so that you can easily see and refer to them. You will also find them attached to the cots and incubators. The cues and scoring will mean the same whether your choice is to breast or formula feeding.
The things you do to help your baby feed well are important
You and your baby’s team will work together to find the best way to feed your baby. Babies in neonatal nurseries may need extra help as they learn to feed. Your baby may need a feeding tube, special feeding position or extra help to breathe comfortably during feeding.
Your baby will guide the pace at which feeding progresses. Babies are individuals and show their unique personality from birth, this means that some babies will show feeding cues early and some babies will show cues later. The timing of your baby’s cues will not delay your baby being ready for home.
It is important to hold your baby close to you when breast or bottle feeding. Spending long periods of cuddling your baby, particularly skin-to-skin holding (also known as Kangaroo Care) has short and long term benefits for both baby and you. We encourage you to be with your baby as much as possible. Please ask about how we can best support you to do this.
We firmly believe that you are the most constant influence in your baby’s life and that your role as a parent is a very significant one at all stages of your baby’s journey. Being with your baby at feeding times is important for progressing to suck feeding. Staff will always available to help you.